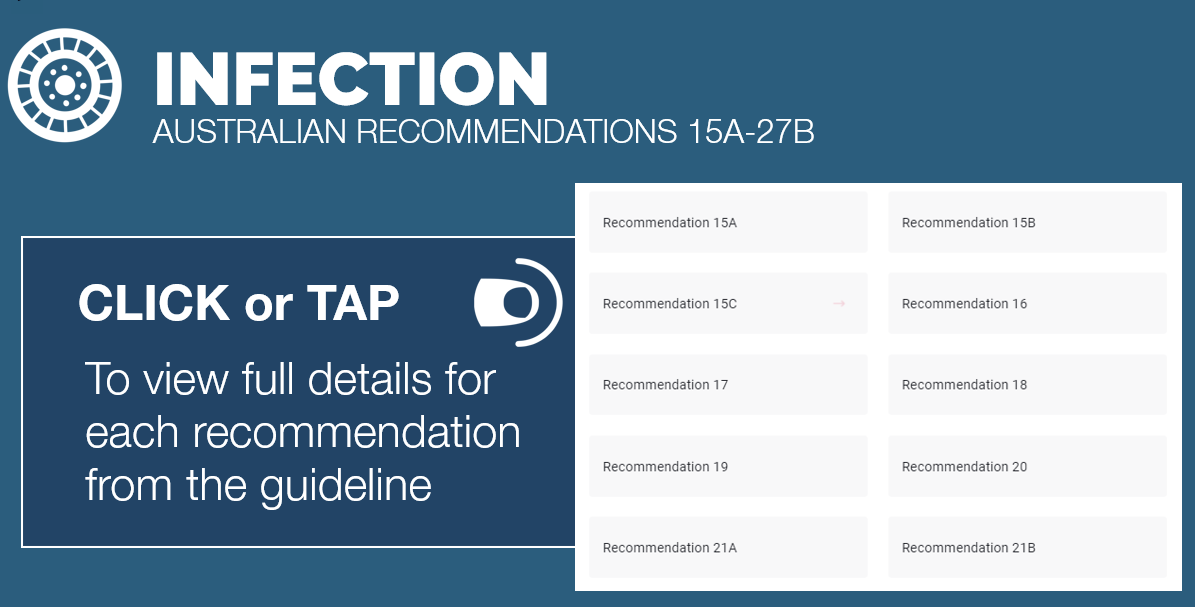
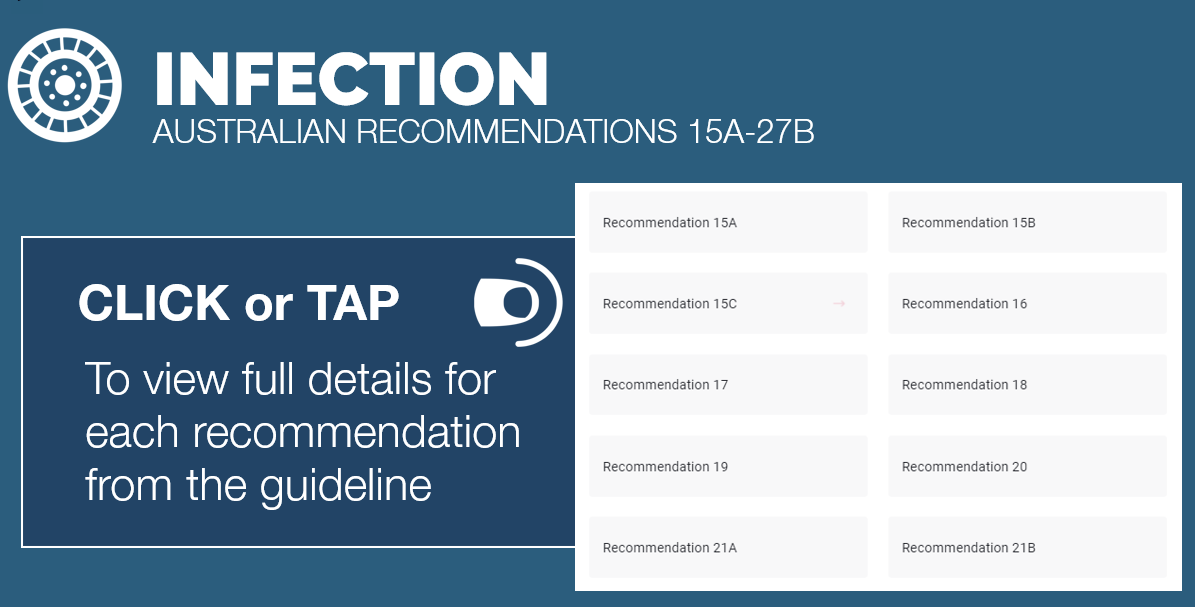
INFECTION RECOMMENDATION LIST (CONT.) | |
RECOMMENDATION 15A | |
Administer antibiotic therapy to a patient with a skin or soft tissue diabetes-related foot infection for a duration of 1 to 2 weeks. (Strong; high) | |
RECOMMENDATION 15B | |
Consider continuing treatment, perhaps for up to 3 to 4 weeks, if the infection is improving but is extensive and is resolving slower than expected or if the patient has severe peripheral artery disease. (Weak; low) | |
RECOMMENDATION 15C | |
If evidence of infection has not resolved after 4 weeks of apparently appropriate therapy, re-evaluate the patient, and reconsider the need for further diagnostic studies or alternative treatments. (Strong; low) | |
RECOMMENDATION 16 | |
For patients who have not recently received antibiotic therapy and have an acute infection, consider targeting empiric antibiotic therapy at just aerobic Gram positive pathogens (beta-haemolytic streptococci and Staphylococcus aureus) in cases of a mild (grade 2) diabetes-related foot infection. (Weak; low) | |
RECOMMENDATION 17 | |
For patients who have been treated with antibiotic therapy within a few weeks, have a chronic infection, have a severely ischaemic affected limb, or a moderate (grade 3) or severe (grade 4) infection, we suggest selecting an empiric antibiotic regimen that covers Gram positive pathogens, commonly isolated Gram negative pathogens, and possibly obligate anaerobes in cases of moderate (grade 3) to severe (grade 4) diabetes-related foot infections. Then, reconsider the antibiotic regimen based on both the clinical response and culture and sensitivity results. (Weak; low) | |
RECOMMENDATION 18 | |
Empiric treatment aimed at Pseudomonas aeruginosa is not usually necessary but consider it if P. aeruginosa has been isolated from cultures of the affected site within the previous few weeks, or in tropical/subtropical climates (at least for moderate (grade 3) or severe (grade 4) infection). (Weak; low) | |
RECOMMENDATION 19 | |
Do not treat clinically uninfected foot ulcers with systemic or local antibiotic therapy with the goal of reducing the risk of infection or promoting ulcer healing. (Strong; low) | |
RECOMMENDATION 20 | |
Non-surgeons should urgently consult with a surgical specialist in cases of severe (grade 4) infection or of moderate (grade 3) infection complicated by extensive gangrene, necrotising infection, signs suggesting deep (below the fascia) abscess or compartment syndrome, or severe lower limb ischaemia. (Strong; low) | |
RECOMMENDATION 21A | |
In a patient with diabetes and uncomplicated forefoot osteomyelitis, for whom there is no other indication for surgical treatment, consider treating with antibiotic therapy without surgical resection of bone. (Strong; moderate) | |
RECOMMENDATION 21B | |
In a patient with probable diabetes-related foot osteomyelitis with concomitant soft tissue infection, urgently evaluate for the need for surgery as well as intensive post-operative medical and surgical follow-up. (Strong; moderate) | |
RECOMMENDATION 22 | |
Select antibiotic agents for treating diabetes-related foot osteomyelitis from among those that have demonstrated efficacy for osteomyelitis in clinical studies. (Strong; low) | |
RECOMMENDATION 23 | |
Treat diabetes-related foot osteomyelitis with antibiotic therapy for just a few days if there is no soft tissue infection and all the infected bone has been surgically removed. (Weak; low) | |
RECOMMENDATION 24 | |
For people with diabetes-related foot osteomyelitis that initially require parenteral therapy, consider switching to an oral antibiotic regimen that has high bioavailability after perhaps 5 to 7 days, if the likely or proven pathogens are susceptible to an available oral agent and the patient has no clinical condition precluding oral therapy. (Weak; moderate | |
RECOMMENDATION 25A | |
During surgery to resect bone for diabetes-related foot osteomyelitis, consider obtaining a specimen of bone for culture (and, if possible, histopathology) at the stump of the resected bone to identify if there is residual bone infection. (Weak; moderate) | |
RECOMMENDATION 25B | |
If an aseptically collected culture specimen obtained during the surgery grows pathogen(s), or if the histology demonstrates osteomyelitis, administer appropriate antibiotic therapy for up to 6 weeks. (Strong; moderate) | |
RECOMMENDATION 26 | |
For a diabetes-related foot infection, do not use hyperbaric oxygen therapy or topical oxygen therapy as an adjunctive treatment if the only indication is specifically for treating the infection. (Weak; low) | |
RECOMMENDATION 27A | |
To specifically address infection in a diabetes-related foot ulcer: do not use adjunctive granulocyte colony stimulating factor treatment (Weak; moderate), and | |
RECOMMENDATION 27B | |
do not routinely use topical antiseptics, silver preparations, honey, bacteriophage therapy, or negative pressure wound therapy (with or without instillation). (Weak; low) |
